What We Can Learn From the COVID-19 Pandemic
Active case numbers vary across the world, with countries like New Zealand hosting no active cases of COVID-19, to the United States who is still struggling with an increasing number of new cases. But how did this come to be? What is the difference in the response and recovery time of these countries and others around the globe? In today’s post, we will be looking into the different global responses of some of the ‘healthiest’ countries in the world and discuss how they were able to mitigate and seemingly recover from COVID-19 so quickly.
Disclaimer: This post will only be speaking on novel measures or efficiency in tactics used to deal with the COVID-19 pandemic. We recognize not all countries have access to the same infrastructure as the ones mentioned in this post. Please think of this post and mentioned methods as a learning point for future application.
New Zealand
Population: 5,002,100
Total Cases: 1,504 (0.03%)
Active Cases: 0
(Data reported from New Zealand’s Ministry of Health, accessed 10 June 2020)
Like most other countries, New Zealand’s pandemic planning had been centered around measures used to mitigate an influenza pandemic. This mitigation model focuses on ‘delaying the arrival of the virus and multiple measures to ‘flatten the curve’ of the pandemic’, however this time around, New Zealand took a different approach; an elimination approach that would employ early lockdown measures, contact tracing, testing, and surveillance.
Though further research is required, scientists look towards response speed; the swift action taken by Prime Minister Jacinda Ardern as a crucial mitigating factor in the spread of COVID-19. The country went into lockdown after reporting only 102 active cases and 0 deaths on 25 March 2020 - a move which was considered early compared to response times that were seen in other nations across the globe. Ardern was key on three mottos: “stay home”, “Be kind”, and “We must go hard, and we must go early”, which resulted in the prevention of an exponential rise in cases
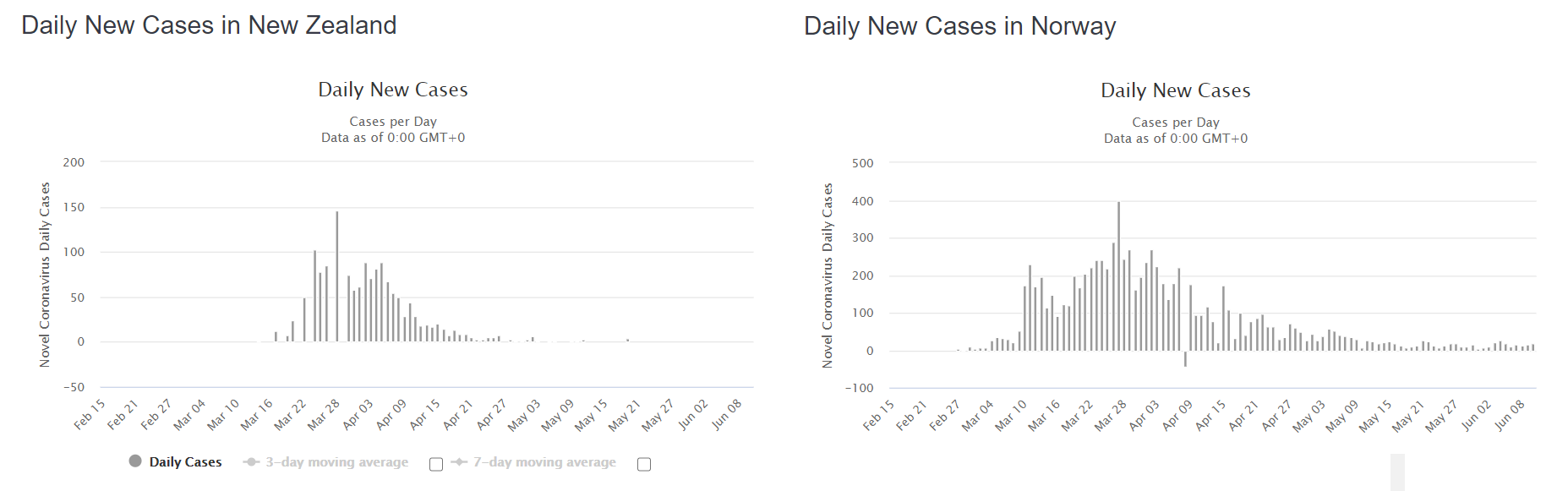
When comparing the daily case data from New Zealand and Norway, there is discrepancy between duration and magnitude of outbreak numbers, though both countries have similar population sizes and infrastructure. New Zealand entered lockdown with only 102 active cases and no COVID-19 related deaths whereas Norway entered lockdown on 12 March 2020, with 800 reported cases and 1 COVID-19 related death. (Data accessed 11 June 2020).
An article quotes the World Health Organization’s Bruce Aylward as saying, “The single best lesson is: speed is everything”, when asked about the response to COVID-19. Due to the swift and strict nature of the country’s lockdown measures, coupled with contact tracing and the usual physical distancing rules, the country is considered to have ‘eliminated’ the virus - which in epidemiological terms means bringing the number of active cases down to zero in a certain geographical area.
South Korea
Population: 51,269,185
Total Cases: 11,947 (0.02%)
Active Cases: 989
(Data from Korea Centers for Disease Control, accessed 11 June 2020)
South Korea’s COVID-19 response was modeled after past outbreak experiences with SARS in 2002, H1N1 in 2009, and most recently MERS in 2015. These disease outbreaks stressed the importance of early testing and prevention of secondary infections from newly infected patients in order to curb the spread. As a result, the country began giving approval for laboratory testing kits which had been previously unapproved, and creating mass numbers of them for use.
By 05 March 2020, the country had already tested 145,000 people - a number larger than the United States, United Kingdom, France, Italy, and Japan combined according to an article by the Atlantic. Mass testing was conducted not only in hospitals, but in drive-through testing stations to reduce crowding and increase hospital capacity for the sick. These stations would provide results within 10 minutes without requiring the patient to leave their car.
To complement their mass testing, South Korea used in-depth monitoring of new cases, also known as contact tracing, which was only possible through their advanced IT system and access to all CCTV. Though there is debate on the legal responsibility and use of this monitoring system, the country was able to track all newly infected individuals and share data on patients that had tested positive for COVID-19. Civilians would receive alerts of where an infected individual had been in a detailed log, and included information such as the infected person’s age, gender, and if they wore a mask in a specific visited area. This information all but included a person’s name, but proved to be effective when case numbers began to drop dramatically in mid-March. This response was only possible through the post-MERS legislation which increased transparency and allowed emergency texts and alerts to be used.
Hong Kong
Despite its close proximity and consistent civilian travel to China, Hong Kong has seen some of the lowest numbers in cases amongst its neighbouring nations. In a region with extremely high population density, some people are left to wonder why Hong Kong’s case numbers are so low.
Articles point towards the preemptive measures taken by the region as border control began on 03 January 2020, a whole 19 days before Hong Kong’s first COVID-19 case was reported on 22 January 2020. Traveler screening, including temperature checks and symptom-related questioning, was implemented at all checkpoints for air or rail travel, and 11 out of 14 border crossings were closed to prevent individuals from already-affected areas of China from entering Hong Kong.
A quick follow-up of closing primary and secondary schools, as well as asking civil servants to work from home on 27 and 29 January 2020 was imposed while numbers were still in the low double digits. Mandatory quarantine was put into place for those in close contact with confirmed cases and the region provided quarantine centers that were composed of retreat centers, camping sites, and new housing estates. Furthermore, on 25 March 2020, all Hong Kong residents required to self-isolate for 14 days were kept under surveillance using electronic wristbands and mobile apps - this ensured compliance with the 14-day quarantine as those breaching orders would be considered to have committed a criminal offence.
What can we take away from this?
In a nutshell, speed, early testing, contact tracing, surveillance, and preemptive measures all played their part in mitigating the spread of COVID-19 in the aforementioned countries and regions. Surely you can find more cases of these examples throughout the globe, but these are just a few that are notably highlighted in current media and that are seen as role models to learn from for those countries still struggling with the pandemic.
This too shall pass - our website’s motto rings true. Though the pandemic has wrought tragedy, there is much to learn in terms of pandemic preparedness, a nod that scientists have given to South Korea and Hong Kong, as their successes lie upon their tragic history with the SARS and MERS outbreaks which took place within the last 2 decades. It is the cooperation of civilian understanding and compliance, and government leadership that can create the best response to a global pandemic that requires teamwork to overcome.
Journal Sources:
https://search.proquest.com/openview/8df823b0b03c0001a580dde662dcec87/1?pq-origsite=gscholar&cbl=1056335
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31097-7/fulltext?utm_medium=social&utm_source=linktress&utm_campaign=how+new+zealand+eliminated+covid-19+the+lancet
https://science.sciencemag.org/content/367/6481/962.full
https://www.nature.com/articles/d41586-020-00740-y
https://www.cmaj.ca/content/192/19/E511
Media Sources:
https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases
https://www.theatlantic.com/ideas/archive/2020/05/whats-south-koreas-secret/611215/
Image Sources:
https://www.theatlantic.com/technology/archive/2020/05/how-hong-kong-beating-coronavirus/611524/
https://time.com/5804899/u-s-coronavirus-needs-follow-s-korea/
https://www.npr.org/sections/coronavirus-live-updates/2020/04/27/845304917/new-zealand-says-it-has-won-battle-against-covid-19
https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases
http://ncov.mohw.go.kr/en/bdBoardList.do?brdId=16&brdGubun=161&dataGubun=&ncvContSeq=&contSeq=&board_id=&gubun=
https://www.cnn.com/2020/03/02/asia/coronavirus-drive-through-south-korea-hnk-intl/index.html
https://www.worldometers.info/coronavirus/country/china-hong-kong-sar/
https://www.nytimes.com/2020/03/13/opinion/coronavirus-best-response.html